Instructions for Clinical Staff
The Academy’s data indicate that aid-in-dying medications can be administered effectively through PEG or other feeding tubes, provided patients undergo proper medical screening, are well-prepared, and receive adequate support. Individualized clinical assessments and attentive bedside care further minimize the risk of complications. Non-oral administration requires specialized clinical expertise, close coordination between the prescribing clinician and bedside teams.
Beyond assessing a patient’s prognosis and decision-making capacity, additional clinical evaluations are necessary to ensure a safe and effective aid-in-dying process for those requiring rectal administration. Bedside clinicians, such as hospice nurses, and recent medical records, including imaging studies, often play a critical role in completing these assessments. Conduct thorough assessments and coordinate with bedside staff:
The effectiveness of aid-in-dying medication relies on intestinal absorption, systemic circulation, and receptor activity. Adequate intake and bowel management should be encouraged to maintain gastrointestinal function. Clinicians should review recent imaging and gastrointestinal evaluations to verify absorptive capacity. Concurrent use of opioids or benzodiazepines should also be assessed, with medication plans adjusted as needed.
Clinical risk factors that may contribute to prolonged death:
When multiple risk factors are present, an increased dosage or alternative aid-in-dying medication regimen or route may be necessary.
See our detailed list of contributing factors here.
Refer to our pharmacology page for dosage guidance.
Please don’t hesitate to contact our hotline if you have questions:
We recommend that prescribers collaborate, when possible, with bedside RNs to gather assessment information and to help determine the dose needed.
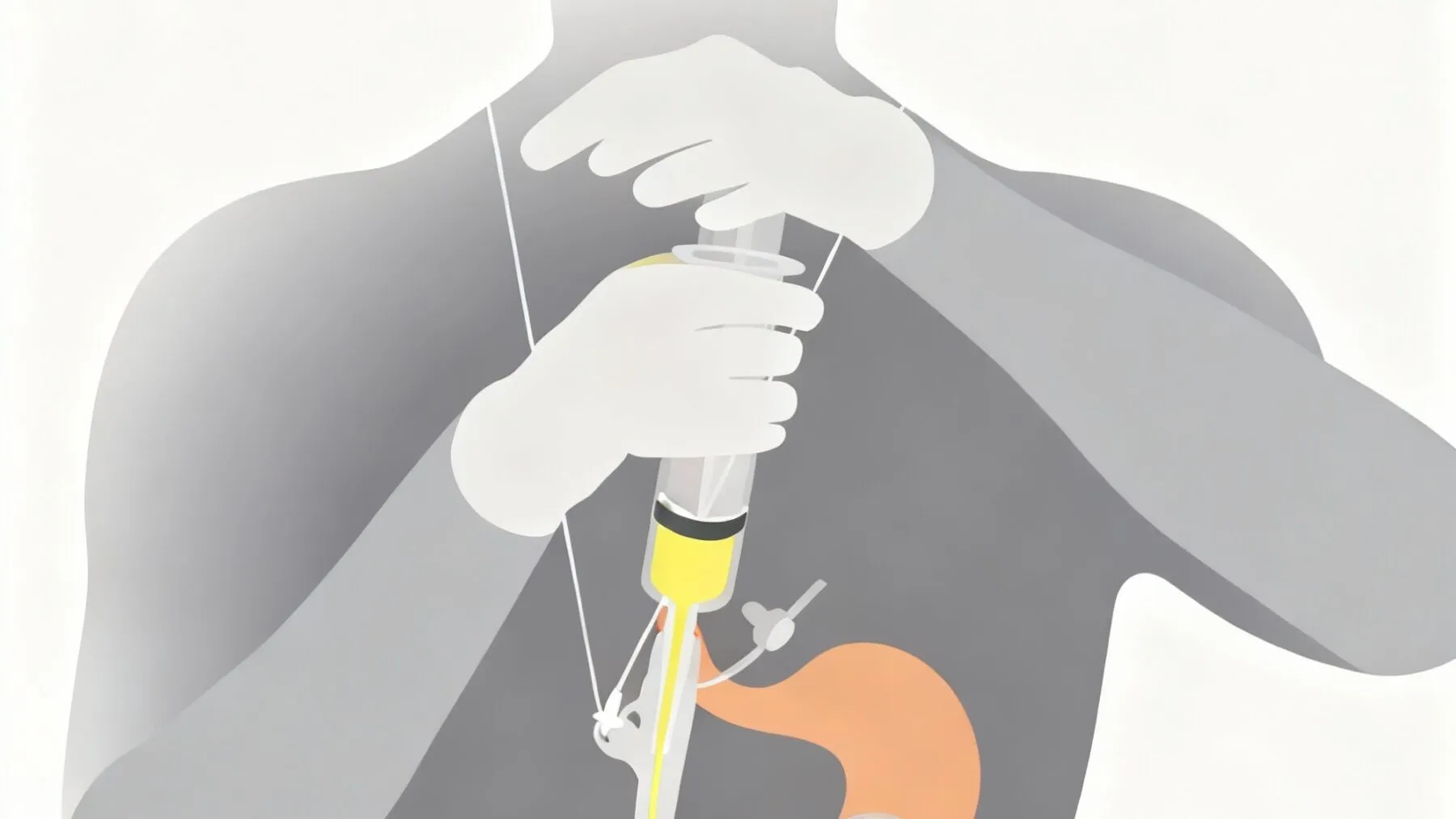
Type of PEG and diameter of the lumen: PEGs with smaller lumens and valves are significantly prone to clogging. If the PEG is a low-profile button style with an anti-reflux valve or has a lumen smaller than 20 Fr, replace it with a standard PEG of 20 Fr or larger to reduce the risk of medication-related occlusions. Avoid using pumps for the aid-in-dying procedure, which carry a high risk of clogging or jamming.
Patient’s ability and preferred method of self-administration: The patient must be able to self-administer 60mL or 100 mL of fluid into their PEG tube by depressing the plunger on a feeding syringe or releasing a clamp, using their teeth or another preferred mechanism. Trial this process before the aid-in-dying day to ensure the patient is able. Avoid using pumps for the aid-in-dying procedure, which carry a high risk of clogging or jamming.
Do not proceed if the patient presents with any of the following:
• Signs of bowel obstruction or gastroparesis, such as uncontrolled nausea, vomiting, not tolerating intake for 24 hrs, no bowel sounds, or no BM in over 5 days.
• Permanent or temporary loss of decision-making capacity
• Insufficient strength to self-administer medication
1. Review patient information: Planning, Preparing, and the Aid-in-Dying Day.
2. The patient should practice their preferred administration method in advance—either by pressing the plunger to completely empty a 60 mL or 100 mL syringe of water into a bowl, or by releasing the clamp on a gravity feeding bag—to ensure they can perform the task easily.
3. Prepare solid contingency plans in case the patient changes plans, loses capacity, or aid in dying becomes clinically inadvisable. These plans should outline who will provide bedside attendant care, the typical signs and symptoms to expect, and medications that might be required.
4. Patients should be encouraged to maintain a sufficient intake to support gastrointestinal motility and absorptive function.
5. Constipation or loose stools should be carefully managed to ensure intestinal motility and absorption. Laxatives or antidiarrheals should be used to ensure the patient produces a soft but formed, easily passed bowel movement approximately every 3-5 days.
6. Nausea and vomiting should also be managed, preferably with non-sedating medications, to support the patient’s capacity.
7. The patient should stop intake after midnight the night before the procedure and consume only clear liquids thereafter.
Tip: Check the prescriber’s order to determine whether a 60 mL or 100 mL catheter-tipped syringe is required:
- 3 x 60mL or 100mL catheter-tipped syringes, with cap. Check the order!
- gravity feeding bag, with clamp (if needed)
- Short glass cup (to mix meds in)
- graduated cylinder (to hold filled syringes upright)
- 8 oz clear filtered apple juice
- PPE: chux, gloves, mask
1. Inspect the medications, confirm the Rx (DDMAPH, patient’s name, and DOB), and ideally put them in the lockbox until needed, for safety.
2. Prepare and update contingency plans with the patient and loved ones, and review what to expect during the procedure.
3. Manage constipation, nausea, or vomiting, and use of comfort medications to optimize GI and cognitive functions.
4. Assess GI function: intake, output, symptoms (Nausea, vomiting, bowel sounds, constipation, diarrhea, ascites), and medications.
5. Assess cognition: orientation, use of comfort or other sedating medications, ability to understand and communicate terminal disease, prognosis, and end-of-life options, including aid-in-dying.
6. Assess the patient’s ability to self-administer by depressing the plunger on a feeding syringe or releasing a clamp, using their teeth or another preferred mechanism.
7. Call the attending provider to review the assessment findings, prescription, and to plan for the procedure.
1. Verbally confirm that the patient wishes to proceed with plans to take the medications to die, and that they understand they can change plans at any time.
2. Ensure all necessary supplies are on hand.
3. Review with the patient and family what to expect on the day of the procedure.
4. Reassess gastrointestinal and cognitive function, and strength/ability to self-administer.
5. Call the attending provider to review the assessment findings and to plan for the procedure.
The day of the planned death, upon arrival:
- Verbally confirm that the patient wishes to proceed with plans to take the medications to die, and that they understand they can change plans at any time, including today.
- Also verbally confirm that they have the ability to self-administer, are sufficiently oriented, and have maintained NPO/clear liquids only after midnight.
- Review what to expect during the procedure.
Review the order, which typically calls for medications to be mixed to a total volume of 60mL or 100mL. Prepare the medications to the total volume ordered, being careful not to overfill the syringe:
1. Choose an uncluttered area, away from others, especially pets or children. Place a barrier, put on masks, and gloves.
2. Draw up and decant roughly ½ to ¾ of the ordered volume (30-50mLs) of clear, filtered apple juice directly into the medication bottle.
3. Cap the bottle and shake it for at least 30 seconds. Check to be sure all the medication is mixed, especially from the bottom of the bottle.
4. Uncap the bottle and pour the suspension from the bottle into a cup, then draw it up into the catheter-tipped syringe.
5. Pour an additional amount of filtered apple juice into the cup and draw it into the syringe, filling it to the total volume ordered, being very careful not to overfill the syringe.
6. Cap the syringe and place it tip/cap-side up into the graduated cylinder, keeping the tip upright to prevent blockage, as medications tend to clump in the tip.
7. Clean up and dispose of any contaminated materials in a plastic bag and store it out of easy reach for later cleanup.
8. Bring capped tip-up medications in the graduated cylinder, along with an additional water-filled catheter-tipped syringe (for pre-flush), to the bedside.
- Have the Patient sit upright or lie on their left side.
- Hold the filled, capped syringe, and shake vigorously for 30 seconds.
- Uncap the syringe and insert it into the catheter.
- Or, pour the medications into the feeding bag and prepare the patient to release the clamp.
- Unclamp the tubing, and anchor the catheter and syringe for the patient if needed.
- Instruct the patient that they may proceed, and depress the plunger or release the clamp.
- Once the patient has self-administered the medications, clamp the line, remove the syringe or feeding bag, and place it in a safe location.
- No further flush is required.
- Note the time of ingestion and the time of full sedation to report later to the attending provider.
- Once sedation has begun, lie the patient down on their left side (to improve absorption).
- Support the family by encouraging them to gather close for comfort, normalize signs of the dying process, and reassure them that the patient is deeply in a coma and is comfortable.
- Once the patient has been unconscious for 30 minutes and the family is settled, consider leaving the bedside to clean up. Gather the syringes, rinse any contaminated containers, including the medication bottle, and remove any labels. Dispose of the bottle, syringes, graduated cylinder, and other contaminated materials in a plastic bag, then place it in the outdoor bin (not in the kitchen trash).
- If staff must depart, family should be notified who to call if they have any questions or concerns, or once the patient has died.
- Death can be confirmed once neck pulses and breathing have stopped for at least 10 minutes.
For questions or immediate assistance:
Contact Thalia DeWolf, RN, CHPN – thalia@aadm.org
or contact the Academy Clinicians Hotline: AADM Clinicians’ Hotline
updated 11/2025